Cardiac System PDF⁚ A Comprehensive Overview
This comprehensive guide explores the intricate anatomy and physiology of the human cardiac system. It delves into the heart’s structure, function, and the vital role it plays in circulatory health. Understanding the cardiac system is crucial for preventing and managing cardiovascular diseases.
Introduction to the Cardiovascular System
The cardiovascular system, also known as the circulatory system, is a vital network responsible for transporting blood throughout the body. This intricate system comprises the heart, a powerful muscular pump, and an extensive network of blood vessels—arteries, veins, and capillaries. Its primary function is to deliver oxygen and essential nutrients to the body’s tissues while simultaneously removing metabolic waste products like carbon dioxide. The ceaseless circulation of blood ensures the maintenance of homeostasis, a state of internal balance crucial for survival. Efficient cardiovascular function is paramount for overall health, as disruptions can lead to various health complications.
The heart, the central component, works tirelessly to propel blood through the pulmonary and systemic circulations. The pulmonary circulation involves the transport of deoxygenated blood to the lungs for oxygenation, while the systemic circulation delivers oxygenated blood to the body’s tissues and organs. The rhythmic contractions of the heart, coupled with the elasticity of blood vessels, ensure the continuous flow of blood, sustaining life’s processes. A thorough understanding of the cardiovascular system’s mechanics is key to appreciating its importance in maintaining overall well-being.
Components of the Cardiovascular System⁚ Heart and Blood Vessels
The cardiovascular system’s primary components are the heart and a vast network of blood vessels. The heart, a muscular organ roughly the size of a fist, acts as the central pump, propelling blood throughout the body. Its four chambers – two atria and two ventricles – work in coordination to ensure efficient blood flow. The right side receives deoxygenated blood from the body and pumps it to the lungs for oxygenation, while the left side receives oxygenated blood from the lungs and pumps it to the rest of the body. This intricate pumping action is regulated by a specialized conduction system within the heart itself.
Blood vessels form a complex network that transports blood throughout the body. Arteries carry oxygenated blood away from the heart, branching into smaller arterioles and ultimately into capillaries, microscopic vessels where gas exchange occurs between blood and tissues. Deoxygenated blood then flows into venules, which converge into larger veins, returning blood to the heart. The structure of blood vessels – arteries with thick, elastic walls for high-pressure blood flow and veins with thinner walls and valves to prevent backflow – reflects their specific functions in the circulatory system. The interplay between the heart and blood vessels maintains a continuous and regulated blood flow essential for life.
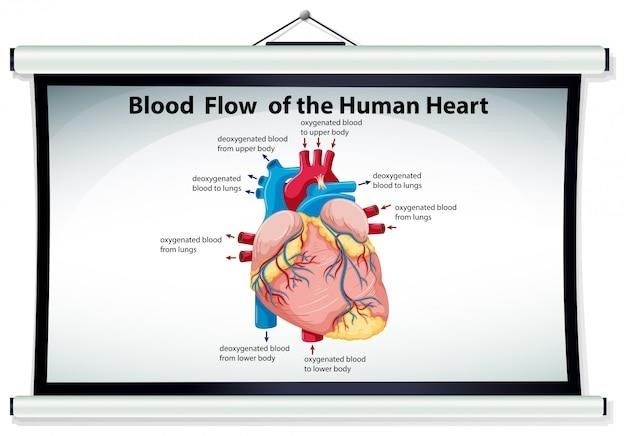
The Pulmonary and Systemic Circuits
The cardiovascular system is organized into two main circulatory pathways⁚ the pulmonary and systemic circuits. The pulmonary circuit is a shorter, lower-pressure loop focused on gas exchange. Deoxygenated blood, collected from the body via the vena cavae, enters the right atrium of the heart. From there, it flows into the right ventricle, which pumps it through the pulmonary artery to the lungs. In the lungs, carbon dioxide is released, and oxygen is absorbed by the blood. This oxygen-rich blood then returns to the heart via the pulmonary veins, entering the left atrium.
The systemic circuit is a much larger, higher-pressure circuit that distributes oxygenated blood to all the body’s tissues and organs. Oxygenated blood from the left atrium flows into the left ventricle, the heart’s most powerful chamber. The left ventricle pumps this blood into the aorta, the body’s largest artery, initiating distribution throughout the body. As blood travels through the systemic arteries, arterioles, and capillaries, oxygen and nutrients are delivered to cells, and waste products, such as carbon dioxide, are collected. This deoxygenated blood then returns to the heart via the veins, completing the systemic circuit and preparing for the next cycle of pulmonary circulation. The continuous interaction between these two circuits ensures efficient oxygen delivery and waste removal throughout the body.
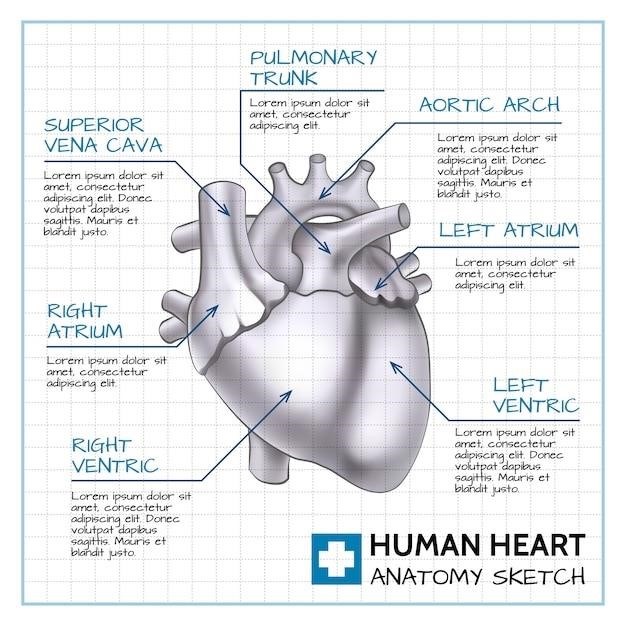
Heart Anatomy⁚ External and Internal Structures
Externally, the heart is a roughly conical organ, approximately the size of a fist, located within the mediastinum of the thoracic cavity. Its apex points inferiorly towards the left, while the base sits superiorly. The heart is enclosed by a double-walled sac, the pericardium, which provides protection and lubrication. The heart wall itself comprises three layers⁚ the epicardium (outermost), myocardium (middle, thickest layer of cardiac muscle), and endocardium (innermost, lining the chambers). The myocardium’s thickness varies significantly between chambers, reflecting their differing workload.
Internally, the heart is divided into four chambers⁚ two atria (receiving chambers) and two ventricles (pumping chambers). The right and left atria are separated by the interatrial septum, while the right and left ventricles are separated by the interventricular septum. One-way valves, the atrioventricular (AV) valves (tricuspid on the right, mitral on the left) and the semilunar valves (pulmonary and aortic), prevent backflow of blood and ensure unidirectional flow. The intricate arrangement of chambers, valves, and associated structures allows the heart to efficiently pump blood through the pulmonary and systemic circuits, sustaining the body’s circulatory needs.
Chambers of the Heart⁚ Atria and Ventricles
The heart’s internal structure is divided into four chambers⁚ two upper atria and two lower ventricles. The right atrium receives deoxygenated blood returning from the body via the superior and inferior vena cavae. This blood then flows through the tricuspid valve into the right ventricle. The right ventricle pumps this deoxygenated blood to the lungs via the pulmonary artery for oxygenation. Meanwhile, the left atrium receives oxygenated blood from the lungs through the pulmonary veins. This oxygen-rich blood passes through the mitral valve into the left ventricle.
The left ventricle, significantly more muscular than the right, pumps the oxygenated blood into the systemic circulation via the aorta. The difference in muscularity reflects the higher pressure required for systemic circulation compared to pulmonary circulation. The atria act as receiving chambers, with thin walls, while the ventricles, particularly the left, possess thicker muscular walls to generate the force needed to propel blood throughout the body. The coordinated contraction and relaxation of these chambers, driven by the heart’s conduction system, ensure the continuous, efficient circulation of blood.
Heart Valves⁚ Structure and Function
The heart’s four valves—tricuspid, pulmonary, mitral, and aortic—ensure unidirectional blood flow. The atrioventricular (AV) valves, the tricuspid (right) and mitral (left), prevent backflow from the ventricles into the atria during ventricular contraction. These valves consist of flaps of tissue, or cusps, that open and close passively in response to pressure changes. The tricuspid valve has three cusps, while the mitral valve has two. Attached to the cusps are chordae tendineae, strong fibrous cords connected to papillary muscles in the ventricular walls. These structures prevent the AV valves from inverting under the high pressure of ventricular contraction.
The semilunar valves, the pulmonary and aortic, prevent backflow from the arteries into the ventricles during ventricular relaxation. These valves are located at the exit points of the ventricles⁚ the pulmonary valve between the right ventricle and pulmonary artery, and the aortic valve between the left ventricle and aorta. Unlike the AV valves, the semilunar valves don’t have chordae tendineae; their structure ensures that they close tightly when the ventricular pressure drops below arterial pressure. The coordinated action of these valves is essential for maintaining the efficient flow of blood through the heart and prevents potentially life-threatening circulatory complications.
The Cardiac Conduction System
The heart’s rhythmic contractions are orchestrated by a specialized conduction system, ensuring coordinated atrial and ventricular activity. This system comprises specialized cardiac muscle cells capable of spontaneously generating and conducting electrical impulses. The sinoatrial (SA) node, the heart’s natural pacemaker, located in the right atrium, initiates the heartbeat by generating electrical impulses. These impulses spread rapidly through the atria, causing atrial contraction. The atrioventricular (AV) node, situated between the atria and ventricles, delays the impulse briefly, allowing the atria to fully empty before ventricular contraction.
From the AV node, the impulse travels down the bundle of His, a specialized conducting pathway that divides into right and left bundle branches extending into the ventricles. The bundle branches further subdivide into Purkinje fibers, a network of fine fibers distributing the impulse throughout the ventricular myocardium, triggering coordinated ventricular contraction. This precisely timed sequence ensures efficient blood ejection from the heart into the pulmonary and systemic circulations. Disruptions to this system can lead to arrhythmias, affecting the heart’s rhythm and potentially causing serious health problems.
Cardiac Muscle⁚ Structure and Function
Cardiac muscle, unique in its structure and function, forms the heart’s walls. Unlike skeletal muscle, cardiac muscle cells, or cardiomyocytes, are branched, striated, and interconnected through intercalated discs. These discs contain gap junctions, facilitating rapid electrical impulse transmission between cells, enabling synchronized contraction. The striated appearance reflects the organized arrangement of sarcomeres, the contractile units containing actin and myosin filaments. The interaction of these filaments, driven by calcium influx, produces the heart’s powerful contractions.
Cardiac muscle exhibits automaticity, the ability to generate its own rhythmic contractions. This inherent rhythmicity is regulated by the cardiac conduction system, ensuring a coordinated heartbeat. Unlike skeletal muscle, cardiac muscle is highly resistant to fatigue, allowing the heart to continuously pump blood throughout life. The unique properties of cardiac muscle, including its branched structure, intercalated discs, and automaticity, are essential for the heart’s efficient and continuous pumping action. Damage to cardiac muscle, as in myocardial infarction, can significantly impair the heart’s function.
Regulation of Blood Pressure
Blood pressure, the force exerted by blood against vessel walls, is meticulously regulated to ensure adequate tissue perfusion. This complex process involves several interacting systems. The baroreceptor reflex, a crucial short-term mechanism, senses pressure changes in major arteries. These specialized receptors send signals to the brainstem, which adjusts sympathetic and parasympathetic nervous system activity to maintain pressure within a narrow range; Increased pressure triggers parasympathetic activation, slowing heart rate and reducing contractility, while decreased pressure stimulates sympathetic activity, increasing heart rate and contractility.
Hormonal regulation plays a vital long-term role in blood pressure control. The renin-angiotensin-aldosterone system (RAAS) is a key player, influencing sodium and water retention, thereby affecting blood volume and pressure. Antidiuretic hormone (ADH) further regulates water balance, impacting blood volume. Other hormones, such as atrial natriuretic peptide (ANP), counter the effects of RAAS by promoting sodium and water excretion. The interplay of these neural and hormonal mechanisms ensures that blood pressure remains stable despite fluctuations in activity, hydration, and other physiological factors. Dysregulation of these systems contributes to hypertension and other cardiovascular diseases.
Coronary Circulation⁚ Blood Supply to the Heart
The heart, a tireless pump, requires its own dedicated circulatory system, the coronary circulation, to deliver oxygen and nutrients and remove metabolic waste. This vital network originates from the aorta, just beyond the aortic valve. The right and left coronary arteries, the main conduits, branch extensively to supply the heart muscle (myocardium). The right coronary artery typically supplies the right atrium and ventricle, along with a portion of the posterior left ventricle. The left coronary artery, dividing into the circumflex and anterior interventricular branches, perfuses the left atrium, the majority of the left ventricle, and the interventricular septum.
Deoxygenated blood, having served the heart muscle, returns via a system of coronary veins, ultimately draining into the coronary sinus, which empties into the right atrium. The intricate branching of the coronary arteries ensures that all parts of the heart receive adequate blood flow. However, blockages within these vessels, often due to atherosclerosis, restrict blood flow, leading to myocardial ischemia and potentially life-threatening conditions like myocardial infarction (heart attack). Maintaining the health of the coronary circulation is paramount for preventing heart disease.
Cardiovascular System Diseases and Conditions
The cardiovascular system, while remarkably resilient, is susceptible to a range of diseases and conditions. Atherosclerosis, the buildup of plaque within arteries, is a primary culprit, narrowing vessels and restricting blood flow. This can lead to coronary artery disease (CAD), where reduced blood supply to the heart muscle causes angina (chest pain) or heart attacks. Hypertension, or high blood pressure, places excessive strain on the heart and blood vessels, increasing the risk of stroke, heart failure, and kidney disease. Heart failure, a condition where the heart can’t pump enough blood to meet the body’s needs, can result from various underlying causes, including CAD and hypertension.
Valvular heart disease involves malfunctioning heart valves, disrupting the normal flow of blood. Congenital heart defects are structural abnormalities present from birth. Arrhythmias, irregular heartbeats, can range from benign to life-threatening. Deep vein thrombosis (DVT), the formation of blood clots in deep veins, often in the legs, poses a risk of pulmonary embolism if the clot travels to the lungs. These conditions highlight the importance of regular checkups, lifestyle modifications, and appropriate medical interventions to maintain cardiovascular health.
Diagnostic Techniques for Cardiovascular Diseases
Diagnosing cardiovascular diseases requires a multifaceted approach utilizing various advanced techniques. Electrocardiograms (ECGs) record the heart’s electrical activity, revealing arrhythmias and other abnormalities in heart rhythm. Echocardiograms utilize ultrasound to visualize the heart’s structure and function, assessing valve function, chamber size, and wall motion. Stress tests evaluate the heart’s response to increased workload, identifying areas of compromised blood flow. Cardiac catheterization, a more invasive procedure, involves inserting a catheter into a blood vessel to directly visualize the coronary arteries and assess for blockages.
Coronary angiography uses contrast dye to highlight the coronary arteries during cardiac catheterization, enabling precise identification of narrowed or blocked vessels. Blood tests, such as lipid panels and cardiac enzyme levels, provide valuable information about cholesterol levels and potential heart damage. Chest X-rays offer a general view of the heart and lungs, detecting abnormalities in size and shape. Magnetic resonance imaging (MRI) and computed tomography (CT) scans provide detailed anatomical images of the heart and surrounding structures, aiding in the diagnosis of various cardiovascular conditions. The choice of diagnostic tests depends on the suspected condition and the individual’s clinical presentation.
Treatment and Management of Cardiovascular Diseases
Treatment strategies for cardiovascular diseases are tailored to the specific condition and its severity. Lifestyle modifications, including dietary changes, regular exercise, and smoking cessation, are cornerstones of management for many conditions. Medications play a crucial role, with options ranging from blood pressure-lowering drugs (antihypertensives) and cholesterol-lowering statins to anticoagulants preventing blood clot formation and antiplatelet agents inhibiting platelet aggregation. For coronary artery disease, percutaneous coronary intervention (PCI), a minimally invasive procedure using balloon angioplasty or stents, may be employed to restore blood flow. In cases of severe blockage or heart failure, coronary artery bypass grafting (CABG), a surgical procedure that creates new pathways for blood flow around blocked arteries, may be necessary.
Heart valve disorders may require surgical repair or replacement, using either mechanical or biological valves. Pacemakers and implantable cardioverter-defibrillators (ICDs) are used to manage heart rhythm problems, providing electrical impulses to regulate heartbeats or deliver shocks to correct life-threatening arrhythmias. Cardiac rehabilitation programs play a significant role in recovery and improving long-term outcomes after cardiac events, incorporating exercise training, education, and psychosocial support. The management of cardiovascular diseases often involves a team approach, with cardiologists, nurses, and other healthcare professionals working collaboratively to provide comprehensive care and improve patient outcomes.